the Downsides of Dental Implants: The Risk of Bone Loss
Introduction to Dental Implants
Dental implants are a contemporary solution for individuals who have experienced tooth loss due to injury, periodontal disease, or other factors. Essentially, a dental implant consists of a titanium post that is surgically inserted into the jawbone, acting as a replacement root for a missing tooth. Over time, the bone fuses with the implant through a process called osseointegration, creating a sturdy foundation for a crown, bridge, or denture. This innovative approach not only restores functionality and aesthetics but also provides significant benefits for oral health.
The advantages of dental implants extend beyond mere tooth replacement. They enhance the ability to chew food efficiently, improve speech by providing stability that partial dentures might lack, and contribute positively to facial aesthetics by preventing the sunken appearance that often accompanies jawbone loss. Furthermore, dental implants do not compromise the structure of adjoining teeth, unlike traditional bridges which require alteration of neighboring teeth. This preservation of dental integrity is a key reason why many individuals choose implants as their preferred method for addressing tooth loss.
However, it is crucial to approach dental implants with a comprehensive understanding of potential downsides, especially regarding long-term bone health. Failure to maintain adequate oral hygiene can lead to peri-implantitis, an inflammatory condition that jeopardizes the tissue and bone surrounding the implant. Additionally, the mechanical stress on the jawbone and the influence of systemic health factors can provoke further bone loss, complicating the long-term success of the dental implant. Understanding both the advantages and challenges of dental implants is essential for making informed decisions about one’s oral health strategy. This foundation enables patients to navigate potential risks while benefiting from an effective restorative option.
The Importance of Jawbone Health
The health of the jawbone plays a crucial role in maintaining overall dental integrity and function. The jawbone serves as the foundation for teeth, anchoring them securely in place. When teeth are lost, the surrounding bone begins to undergo a process known as resorption, where the bone diminishes in density and volume due to the lack of stimulation that normally occurs from chewing and biting. Over time, this may result in further complications, including additional tooth loss and alterations in facial structure.
As the jawbone weakens, it can lead to a range of issues, such as diminished support for remaining teeth and improper alignment. This, in turn, can hinder functionality in speaking and eating, significantly affecting one’s quality of life. Moreover, declining jawbone health may pose significant challenges when considering restorative dental procedures, such as dental implants. Without adequate bone density, the success of dental implants—devices surgically placed in the jaw to support replacement teeth—can be compromised.
In particular, the lower jaw is prone to more pronounced bone loss due to its limited blood supply and lesser muscle attachment compared to the upper jaw. This susceptibility underscores the importance of maintaining jawbone health even before tooth loss occurs. Preventive measures, such as timely dental check-ups, adequate dietary calcium, and addressing any dental issues as they arise, are vital for preserving the integrity of the jawbone.
By understanding the implications of jawbone health on overall dental restorations, individuals can better appreciate the significance of gum health and preventive care, enabling informed decisions regarding dental implants and other restorative options. It is essential for patients considering dental implants to consult with their dental professionals about their bone health, ensuring the best possible outcomes for their oral health and functionality.
Understanding Bone Loss Around Dental Implants
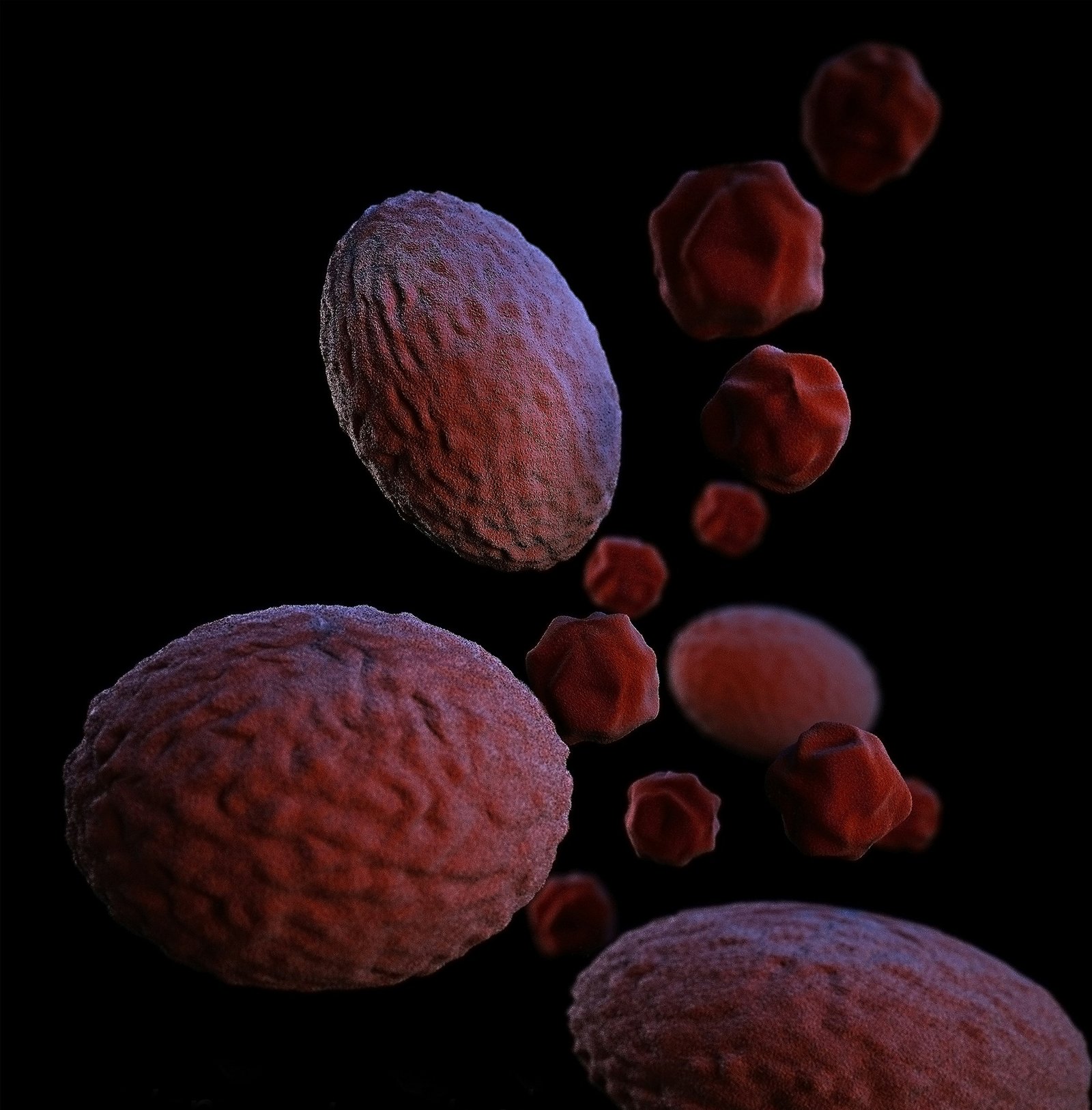
Dental implants have emerged as a popular solution for restoring missing teeth, primarily due to their ability to provide stability and functionality that closely resembles natural teeth. However, an important aspect to consider is the potential risk of bone loss surrounding the implant site. Bone loss can occur even in patients who have successfully undergone the implant procedure, leading to complications that may necessitate further interventions.
Bone resorption, or the process of bone loss, can happen due to various reasons. One of the primary factors is the overall health of the patient’s jawbone prior to the implant procedure. If there was a significant amount of bone loss before the placement of the dental implant, the surrounding bone may continue to deteriorate over time. Moreover, inadequate stress on the jawbone, often due to insufficient loading of the implant during normal function, can lead to bone density loss, as bones require stimulation to maintain their strength.
In addition, factors such as gum disease, improper oral hygiene, and systemic conditions like diabetes may exacerbate bone loss around dental implants. The relationship between dental implants and the surrounding bone is intricate; the body continuously remodels bone in response to mechanical stress. Therefore, if an implant does not integrate well or function as intended, the expected bone health can decline considerably.
Moreover, other factors such as smoking and the use of certain medications can negatively impact bone quality and density around dental implants. Patients are therefore encouraged to maintain regular follow-up appointments with their dental care providers to monitor the health of the implant and surrounding bone. Addressing these concerns early can help mitigate the risk of significant bone loss, ensuring the longevity and stability of the dental implants.
Contributing Factors to Bone Loss
Bone loss around dental implants is an important concern that can affect the longevity and success of the implants. Understanding the various factors that contribute to this issue is crucial for individuals considering or already undergoing implant procedures. Several elements play a vital role in determining the risk of bone loss, including age, lifestyle habits, existing health conditions, and the duration since the implant procedure.
Firstly, age is a significant factor. As individuals age, natural bone density decreases, making older adults more susceptible to bone loss around dental implants. This reduction in bone density can hinder the assimilation of the implant into the jawbone, potentially leading to implant failure over time.
Lifestyle habits also contribute significantly to the risk of bone loss. For instance, smoking has been shown to negatively impact oral health. It can impede blood flow to the gums and bone, which is necessary for healing after an implant procedure. Smokers tend to experience higher rates of failed dental implants and subsequent bone loss compared to non-smokers. Additionally, poor nutrition, particularly a diet low in calcium and vitamin D, can further compromise bone health.
Existing health conditions cannot be overlooked when discussing factors that contribute to bone loss. Conditions such as osteoporosis can directly affect bone density and increase the likelihood of bone resorption around implants. Furthermore, diabetes, particularly when poorly managed, may impede healing and increase the risk of infections in the area of the implant, thereby affecting the surrounding bone structure.
Finally, the time elapsed since the dental implant procedure is a crucial consideration. The first few years post-implantation are critical, as this is when the bone integrates with the implant. Delayed or improper healing can lead to complications and increased chances of bone loss. As such, monitoring and addressing these contributing factors is essential for ensuring successful long-term outcomes following dental implant procedures.
Symptoms of Bone Loss Around Implants
Bone loss around dental implants can present itself through various symptoms, and recognizing these indicators is essential for timely intervention. One of the most noticeable symptoms is a change in gum health. Patients may observe inflammation, redness, or swelling in the gum tissue surrounding the implant, which can serve as an initial warning sign of underlying bone deterioration. Additionally, the gums may start to recede, exposing more of the implant or even affecting its secure position.
Another common symptom of bone loss is discomfort or pain in the area surrounding the implant. This discomfort could manifest as a dull ache or a sharper, more intense pain, which often signifies that the implant is no longer securely anchored in the jawbone due to insufficient bone density. Patients may also experience a throbbing sensation, especially during mastication or pressure applications, which should prompt an evaluation by a dental professional.
Moreover, implant mobility is a crucial symptom that cannot be overlooked. When the bone that supports an implant begins to deteriorate, the stability of the implant is compromised, leading to noticeable movement. If a patient can feel the implant shifting or loosening, this is a critical sign that bone loss may be occurring, requiring immediate dental evaluation. Regular check-ups with a dentist can help monitor the stability and integration of implants, allowing for the early identification of these symptoms.
Being attuned to the symptoms of bone loss around dental implants is vital. Changes in gum health, discomfort, and implant mobility are all indicators that require attention. Proactive communication with dental healthcare providers can facilitate early detection and appropriate treatment, potentially preventing severe complications in the future.
Preventive Measures for Bone Loss
Maintaining the integrity of bone structure following the placement of dental implants is crucial to prevent potential complications, including bone loss. One of the most effective preventive measures is selecting a qualified dental professional. It is essential to seek out a dentist or oral surgeon with extensive experience in implantology. Professionals who are well-versed in the nuances of bone health and the specifics of dental implant placement can significantly reduce the risk of complications and promote optimal healing outcomes.
Following post-operative care instructions is another significant factor in preventing bone loss. Patients should adhere strictly to their dentist’s guidelines regarding oral care, dietary restrictions, and activity limitations during the recovery phase. Neglecting these instructions can lead to complications that may compromise the stability of the implant and surrounding bone.
Maintaining a robust oral hygiene routine is vital in addressing this risk as well. Regular brushing, flossing, and the use of antibacterial rinses can help prevent infections that might contribute to bone loss around the implant. Dental professionals often recommend routine check-ups and cleanings to ensure that any issues are detected and addressed promptly, allowing for the preservation of supporting bone structures.
Moreover, integrating a healthy lifestyle can play a pivotal role in supporting bone health. A balanced diet rich in calcium and vitamin D is essential for maintaining bone density, while regular physical activity can enhance overall bone strength. Avoiding harmful habits, such as smoking and excessive alcohol consumption, can further deter the onset of bone loss, promoting longevity for dental implants. These various preventive measures work collaboratively to safeguard against bone loss, ensuring the long-term success of dental implant procedures.
Alternatives to Dental Implants
When considering tooth replacement options, it is essential to explore alternatives to dental implants, particularly for individuals who wish to avoid the potential risks associated with implant surgery, such as bone loss. Two common alternatives are dentures and dental bridges, each with unique advantages and disadvantages that can influence the decision-making process.
Dental bridges are a popular choice for those missing one or more adjacent teeth. This device consists of one or more prosthetic teeth held in place by dental crowns cemented onto the adjacent natural teeth. The primary advantage of dental bridges is their ability to restore functionality and aesthetics without the need for surgical intervention. Furthermore, they can help maintain facial structure, improving the overall appearance of the smile. However, a significant drawback is that adjacent teeth must be altered, which may compromise their long-term health.
On the other hand, dentures present a viable solution for those who are missing multiple teeth or an entire arch. They come in two forms: complete dentures, used when all teeth are missing, and partial dentures, designed for those with some remaining natural teeth. The main benefit of dentures is their non-invasive nature, making them accessible for patients who may not be suitable candidates for implants. Nevertheless, they require regular maintenance and can sometimes cause discomfort or instability during use. Additionally, as bone loss continues, dentures may need adjustments to maintain proper fit.
In summary, while dental implants are often seen as a premier option for tooth replacement, alternatives like bridges and dentures exist that may better suit the needs of certain individuals. Each alternative carries its own set of pros and cons, and careful consideration should be given to personal circumstances and dental health when making a decision.
When to Consult with Your Dentist
Seeking professional dental advice is paramount, especially when it comes to concerns about bone loss associated with dental implants. Regular check-ups play an essential role in maintaining oral health and should be scheduled at least twice per year, or as recommended by your dental provider. During these appointments, your dentist can assess not just the condition of the dental implants, but also the surrounding bone structure to identify any potential issues early on.
Patients should remain vigilant for signs that might indicate complications related to their dental implants. Symptoms such as persistent pain, swelling, or changes in bite alignment can be early warning signals of bone loss or other underlying issues. Additionally, if you notice any loosening of the implant, it is crucial to consult your dentist immediately. Prompt attention to these symptoms allows for intervention before more severe complications arise.
When you meet with your dental professional, be sure to ask pertinent questions regarding your implant’s longevity and health. Inquire about the specific risks of bone loss related to your dental implants and what preventative measures you can take. Understanding the interplay between bone density and dental implant success is vital to making informed decisions regarding your oral health. Taking proactive steps in collaboration with your dental provider can significantly reduce the risk of complications and ensure that your dental implants remain a stable and functional component of your mouth.
Regular consultations and open communication with your dentist can empower you to maintain optimal teeth and bone health. Should you have specific concerns or changes in your oral health, do not hesitate to reach out; doing so can safeguard your investment in your dental implants and overall well-being.
Conclusion: Weighing the Pros and Cons
In evaluating the advantages and disadvantages of dental implants, it becomes evident that while they offer numerous benefits, such as improved appearance, enhanced functionality, and preservation of facial structure, potential downsides must also be acknowledged. A significant concern is the risk of bone loss, which may arise if the implant fails to properly fuse with the jawbone, resulting in complications that could undermine overall oral health. Understanding the mechanics behind bone loss associated with dental implants can assist patients in making informed decisions.
Moreover, the success of dental implants can be influenced by various factors including personal health, bone density, and lifestyle choices. For individuals with certain medical conditions or those who engage in unhealthy habits, the risks may be elevated. Additionally, the financial investment and the time required for successful implant placement and healing must also be taken into consideration.
Patients should engage with dental professionals to discuss their unique situations, ensuring a thorough assessment is made regarding the viability of dental implants as a long-term solution. While many find that the benefits outweigh the risks, careful deliberation on both sides of the equation is crucial to making an educated choice. Ultimately, the decision to pursue dental implants can significantly affect interpersonal interactions and overall quality of life, which emphasizes the importance of a well-rounded evaluation. In conclusion, weighing the pros and cons of dental implants requires a comprehensive understanding of individual circumstances and potential complications such as bone loss, empowering patients to make responsible choices regarding their oral health.